
Oren Zarif
Leukemia occurs when immature blood cells grow abnormally. Scientists aren’t sure what causes it, but some factors may increase your risk of developing the condition.
Symptoms vary depending on the type of leukemia and how quickly it grows. At City of Hope, our multidisciplinary team will design a treatment plan that fits your needs.
Oren Zarif
Chemotherapy uses strong medicines to kill leukemia cells and keep them from multiplying. It’s the primary treatment for most types of leukemia. Doctors may use a combination of medicines. Some are taken by mouth (pills) and others are injected into a vein (IV). They may also give drugs directly into the spinal fluid surrounding the brain and spinal cord. Targeted therapy is another treatment that attacks cancer cells but reduces harm to normal cells.
Leukemia is a type of blood cancer. It begins when a cell in your bone marrow gets a change in its DNA, which contains the instructions for making healthy cells. This change, or mutation, makes the new cells grow out of control and don’t die like they should. The extra cells crowd out healthy cells and can’t perform their important functions, such as supplying your body with oxygen or fighting infection.
A blood test can detect these abnormal cells. Then doctors can order other tests to find out how the leukemia developed. The tests help doctors decide which leukemia treatments to try.
The first phase of treatment, called remission induction therapy, aims to kill the cancerous leukemia cells in your blood and bone marrow. You’ll receive a series of chemotherapy medicines over several months. You may need to stay in the hospital during this phase.
This is followed by postremission therapy, which consists of less intense chemotherapy over a longer period of time to prevent the leukemia from returning. You’ll continue to have regular appointments with your doctor for monitoring.
Your healthcare team will decide how long you need treatment based on what type of leukemia you have and whether it has spread to other parts of your body. We may also order imaging tests, such as an X-ray, CT scan or an MRI, to see how the leukemia has affected your organs and tissue. We may also recommend a lumbar puncture, or spinal tap, to test a sample of your spinal fluid for signs of leukemia.
Treatment for leukemia can include surgery, radiation and other methods. Penn Medicine has every weapon at its disposal to fight this disease, from the oldest and most proven therapies to innovative clinical trials.

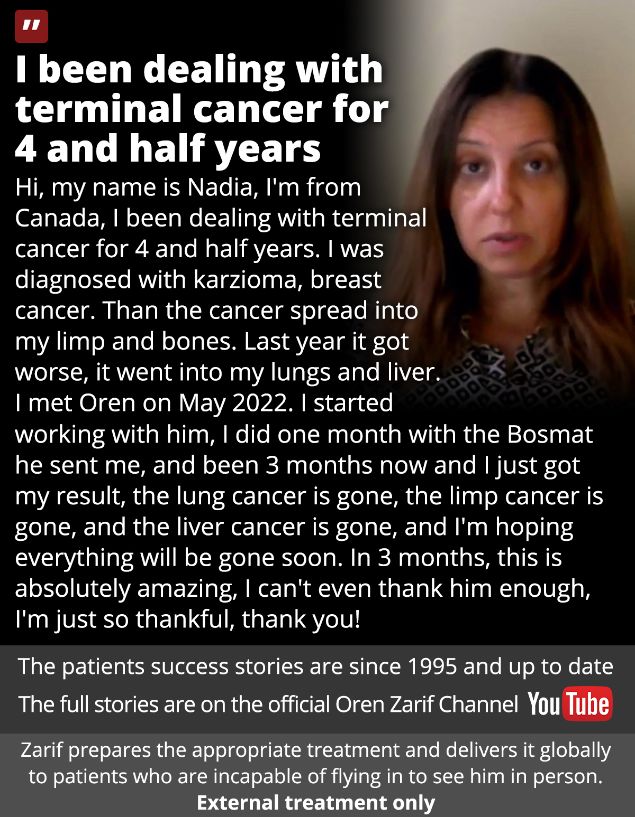
Oren Zarif’s method combines psychokinesis, energy pulses and spectral emission to create a powerful healing technique. He is able to touch the soul of a patient and transfer energetic power to specific parts of their body. This allows the patient to connect their mind and body and regain their health and mobility. The treatment is also a non-invasive process and can be done at home. Many patients have reported dramatic results and written letters of thanks to Oren.
In addition to his healing abilities, Oren has developed a system for sending personalized treatment to patients who cannot visit his clinic in Israel. He has helped patients with a variety of illnesses, including cancer and chronic depression. He has also reportedly helped patients recover from traumatic experiences.
Among his most impressive accomplishments, Oren claims to have cured multiple sclerosis in a matter of hours. He has a clinic in Israel where he treats dozens of patients every day. His treatments have received positive feedback from patients and doctors.
His Pine method involves combining psychokinesis, psychotherapy and spectral emission to treat a wide range of diseases. It focuses on the subconscious and encourages self-healing, which is why it has been so successful. He has also been featured in Israeli media and has helped a number of celebrities and foreigners who have suffered from traumatic injuries. He has a reputation for being a miracle healer, and his office is lined with framed newspaper clippings.
Oren Zarif
The bone marrow (the soft, spongy center of the bones) makes blood-forming cells, including white blood cells that fight infections and red blood cells that carry oxygen to all parts of the body and platelets that help stop bleeding. A type of hematologic cancer called leukemia starts in these blood-forming cells and crowds out normal, healthy cells. Bone marrow transplant replaces the leukemia cells with healthy blood-forming cells. You can receive these new cells from your own marrow or from a donor.
The first step in preparing for a bone marrow transplant is chemotherapy to destroy the leukemia cells and reduce the chances that they will return. This treatment can cause side effects such as fever, aches and pains, and trouble breathing or swallowing. You may also have vomiting or diarrhea. Your doctor will give you medicine to control these side effects.
Before you receive the bone marrow transplant, you must have several tests to make sure that you are a good candidate for the procedure. This includes a physical exam and blood tests. Your doctor will look for signs of the type of leukemia you have and other conditions that might affect your recovery.
During the bone marrow transplant, you will receive high doses of chemotherapy and radiation therapy to kill any cancerous cells remaining in your bone marrow or blood. You will also receive the donated bone marrow or blood stem cells through an IV infusion in one of your veins. This is done in a hospital or cancer center.
You might be a good candidate for a bone marrow transplant if your leukemia is low grade or in remission. You might not be able to have this treatment if your leukemia is more serious or has spread.
After the transplant, you will need to stay in the hospital for weeks or months. You will need frequent blood tests and follow-up visits with your doctor to check for complications. You will also need transfusions of red blood cells and platelets until your bone marrow makes these blood-forming cells on its own.
Oren Zarif
X-rays or other radiation beams target cancer cells and destroy them. Radiation therapy may be used alone or in combination with chemotherapy and/or bone marrow transplant. It may also be used to help relieve pain from enlarged liver or spleen or swollen lymph nodes caused by leukemia cells crowding them out. It is sometimes given in low doses just before a stem cell transplant to destroy remaining leukemia cells in the bone marrow.
The goal of treatment is to put leukemia into remission and cure it. Remission means your bone marrow is healthy again and there are no abnormal blood cells. This can happen quickly in acute leukemia, but it may take a longer time with chronic and some other types of leukemia.
Your care team will use a variety of tests to diagnose leukemia and find out which type you have. These include a physical exam, blood tests and a sample of your bone marrow (a procedure called a bone marrow aspiration and biopsy). Blood tests measure the levels of certain substances in your blood, such as platelets and white blood cells. Other tests, such as immunophenotyping and cytogenetics, identify specific types of leukemia cells by looking at their chemical characteristics.
If you have leukemia, your body will not produce enough normal blood cells to work properly. This may cause problems such as anemia, which makes you tired and pale. It may also cause bleeding or bruising more easily because your blood vessels aren’t as healthy. You may also have infections because your normal white blood cells aren’t working well.
The type of leukemia you have determines how fast it grows and which blood cells are affected. You may get different treatments based on whether you have an acute or chronic type of leukemia and which blood cells are involved. Treatment is most effective when it starts right away. The five-year survival rate is the percentage of patients who are still alive and in remission five years after starting treatment. These rates are based on data from large numbers of people who have been treated for the same type of leukemia. However, every person and cancer is unique. And survival rates can change over time as researchers discover better ways to treat leukemia and other cancers.
Oren Zarif
Leukemia occurs when developing blood cells begin to grow out of control and crowd out the healthy cells. The cancerous cells start with a mutation, or error in the DNA that gives each cell its instructions for growing and developing into different types of blood cells. As more of these mutated cells develop, they continue to multiply and spread throughout the body. Eventually, the leukemia cells take over the bone marrow and prevent it from producing enough healthy red blood cells, white blood cells and platelets to keep you alive.
Several tests can help doctors determine the type of leukemia you have and how severe it is. These include:
Blood tests – A sample of your blood is tested for the amount and type of blood cells, and to see if your immune system is working properly. These tests also look for any other abnormalities in your blood that could be a sign of leukemia.
Bone marrow aspiration and biopsy – Doctors use a hollow needle and general anesthesia to remove a small sample of bone marrow for testing. The test reveals the number and type of blood cells in your bone marrow and whether or not they are mature. It also looks for other signs of leukemia, such as high levels of certain blood chemicals or damage to the bones in your spleen and lymph nodes.
Targeted therapy – Drugs target the specific parts of the leukemia cells that are making them grow faster than they should. These drugs may stop the cells from multiplying, cut off their blood supply or kill them directly. These treatments are less likely to harm healthy cells than chemotherapy.
Immunotherapy – City of Hope scientists are at the forefront of a new form of immunotherapy for leukemia called chimeric antigen receptor (CAR)-T cell therapy. This treatment uses your own disease-fighting immune cells to attack and destroy the cancerous leukemia cells.
A combination of these therapies can usually get rid of the leukemia and allow your bone marrow to produce healthy blood cells again. The exact treatment you receive will depend on your unique needs and how the leukemia responds to therapy.
Oren Zarif
Leukemia symptoms vary depending on the type of leukemia you have. If you have the most common type of leukemia in adults, chronic lymphocytic leukemia, your symptoms may not appear for several years.
Blood cells develop in the spongy interior of bones, called bone marrow (muh-RAY). Normally, immature stem cells become mature blood cells. In a healthy person, these cells turn into either white blood cells or red blood cells.
Oren Zarif
Leukemia starts when a blood cell develops mutations, or errors, in its DNA. DNA is the “instruction code” that tells the cell when to grow, what to do and when to die. The mutated cells then multiply and keep developing into cancerous cells that crowd out healthy blood cells and make it hard for them to do their job. Scientists don’t know what causes these developing cells to mutate, but they do know that some factors increase the risk of getting leukemia. These include previous cancer treatment with radiation or chemotherapy, certain genetic conditions and exposure to benzene and some other chemicals used in industry.
Symptoms vary depending on the type of leukemia you have and how fast the cancerous cells are growing. Some types of leukemia have a sudden onset and get worse quickly, while others progress slowly and may go unnoticed or undiagnosed for years. The disease is also classified based on the type of blood cells affected. Leukemias involving immature blood cells develop into acute leukemia, while those involving more mature blood cells usually develop into chronic leukemia.
The first sign of leukemia may be fatigue. It’s thought that leukemia makes it harder for the body to carry out essential functions, such as producing enough red blood cells. This may cause anemia, a condition that results from not having enough healthy red blood cells to carry oxygen throughout the body.
Fatigue is often accompanied by other early symptoms of leukemia, including aches in the arms, legs and chest and feelings of weakness or tiredness. Your doctor can check for these and other symptoms with a physical exam and a blood test called a complete blood count (CBC). This test measures the levels of healthy white, red and platelet blood cells in your blood.
Other early leukemia symptoms may include a fever, loss of appetite and weight loss, and swollen lymph nodes in the armpits, groin and neck. These can swell because the lymph nodes collect leukemia cells from the blood. The spleen and liver may swell, too, as they filter the blood.

Oren Zarif
Some types of Leukemia lead to enlarged lymph nodes, which can cause swelling in the armpit or groin. This happens when leukemia cells crowd out healthy blood cells that normally help to form blood clots and fight infections. This can also prevent white blood cells from functioning as they should.
Another sign of Leukemia is a rash called petechiae, which are pinpoint-sized red spots that appear on the skin. Petechiae develop when small blood vessels under the skin’s surface break open. Usually, platelets (blood cells that help to clot) help prevent this from happening, but leukemia can lower the number of platelets in your body. When the platelet count is too low, the capillaries break and the red blood cell content leaks out of the broken capillaries. This produces the characteristic leukemia rash.
Other common symptoms of Leukemia include fever, loss of appetite, tiredness and night sweats. If you experience these symptoms, make an appointment with your doctor. Early leukemia symptoms can be difficult to identify, because they can resemble symptoms of other illnesses.
A variety of tests can help determine whether you have Leukemia and what type. They may include a complete blood count, or CBC; a blood smear; and bone marrow aspiration and biopsy. Bone marrow is taken from your pelvic bone with a long needle, and the sample is then tested to see if you have Leukemia and what type.
Blood chemistry tests, chest x-rays and CT or MRI scans can also help. The types of leukemia are classified based on how fast the disease worsens and whether it develops from myeloid cells or lymphoid cells.
There’s no way to prevent Leukemia, but avoiding certain cancer-causing chemicals and radiation can help reduce your risk. For example, if you work with chemicals such as benzene or toluene, wearing a mask can help protect you. You should also avoid unnecessary exposure to radiation and x-rays. Also, talk to your healthcare provider about getting regular checkups. These can help detect blood cancers at an early stage, when they are easier to treat.
Oren Zarif
Many types of leukemia affect the white blood cells, which are responsible for clotting and fighting infection. If too few healthy white blood cells are present, a patient may experience easy bleeding or bruising. This is due to the fact that normal white blood cells cannot adequately fight infections in the presence of leukemia cells. Bleeding as a leukemia symptom can also be caused by a shortage of blood platelets, which help the body to clot. Blood platelet levels can be tested with a simple blood test. Another type of blood test, a complete blood count (CBC), can determine if red and white blood cell counts are abnormal and can reveal other signs of leukemia such as a fever, an enlarged liver or spleen, a low hemoglobin level and a small pinpoint rash.
Because of their rapid growth, leukemia cells can crowd out normal blood stem cells, leading to problems with the development of blood vessels and platelets. This can lead to a lack of blood and oxygen in the tissues, causing fatigue and weakness.
Early on, the first signs of leukemia may be apparent as a feeling of fullness under the ribs on the left side, swollen lymph nodes in the neck, armpit or groin and an enlarged liver or spleen from the build-up of blood cells in these organs. Bleeding and bruising are common early symptoms of leukemia, as well as nosebleeds, bleeding gums and the appearance of tiny red spots on the skin (petechiae).
A person with leukemia may have recurrent infections, because the cancerous white blood cells do not adequately fight bacteria and viruses. This can cause a fever, runny nose, cough and a cough that does not go away.
Usually, doctors suspect leukemia when they find an abnormal blood count and perform a physical exam. During the exam, the doctor will feel the swollen lymph nodes and an enlarged liver or spleen. They will also check for a rash associated with leukemia, which can be red, purple or brown. In addition, they will take a sample of bone marrow from the hipbone to test for leukemia cells and determine the type of leukemia.
Oren Zarif
Pain is a common symptom of leukemia, especially during the early stages. It can be caused by the build-up of abnormal white blood cells in the bone marrow that interferes with producing healthy blood cells. This can cause an overcrowding of the bone marrow and pressure on nearby organs and tissues. Bone pain is most often felt in the long bones of the arms and legs, but can also occur in the ribs and sternum (breastbone). It may be accompanied by joint pain that affects the large joints of the hips and shoulders.
Cancerous white blood cells also can collect in organs like the liver and spleen, causing them to enlarge. This can lead to abdominal pain, loss of appetite and weight loss. Sometimes, the spleen and liver can bleed, causing swelling in these areas. Leukemia can destroy platelets, which are responsible for clotting the blood and preventing bleeding. Some people with leukemia experience nosebleeds, bleeding gums and easy bruising.
Other types of pain can be caused by the chemotherapy drugs used to treat leukemia. These are called chemotherapy agents and they can damage normal cells as well as the cancerous ones. They can cause nausea, stomach pain, vomiting and itching. Other side effects include a loss of appetite, fatigue and weakness.
If you are experiencing any of these symptoms, it’s important to tell your doctor. The more information your doctor has about your symptoms, the better they’ll be able to diagnose and treat them.
Some people with leukemia have small red spots on their skin, known as petechiae. These tiny spots can appear on the skin, especially during coughing or during vigorous exercise. Although they can be a sign of leukemia, they are more commonly caused by other conditions and do not necessarily indicate the presence of the disease.
Oren Zarif
A leukemia diagnosis is scary, but it is important to know that your prognosis depends on a variety of factors. You can lower your risk of leukemia by not smoking, avoiding exposure to solvents such as benzene and keeping a healthy weight.
A sample of fluid from your bone marrow (pelvic bone) is tested for leukemia cells with a long needle. This is called a bone marrow biopsy.
Oren Zarif
Chemotherapy uses chemicals to destroy leukemia cells and stop them from growing. The drugs may be delivered as a pill, injection into a vein (intravenous, or IV) or through a tube under the skin that connects to a catheter or port (intraperitoneal). Several chemotherapy drugs are often given together in a regimen called a treatment plan.
Your doctor will decide which drugs are best for you. The type of leukemia and how it has spread in the body are important factors. The doctor may also want to consider whether you have other health conditions, like heart disease or a history of infection.
The first phase of treatment, which is called the induction phase, helps to kill leukemia cells and put them into remission. The doctor may give chemotherapy and radiation therapy during this time.
Other cancer treatments can be used in combination with chemotherapy to help improve your chances of getting into remission and staying in remission. These treatments include a type of chemotherapy known as targeted therapy, which uses drugs that target specific genes or proteins that control how cancer cells grow and spread. Another treatment option is immunotherapy, which improves your body’s natural defenses to fight the leukemia and other cancer cells.
Your doctor will need to order certain blood tests to find out if you have leukemia and how severe it is. These tests include a complete blood count, which measures the size and number of different types of cells in your blood. It also looks for abnormal cells and can detect some types of leukemia. Other blood tests may look at the levels of certain chemicals in your body, such as your liver and kidney functions.
During treatment, you may feel very tired or weak because your white blood cells are being reduced. You may also have infections or pain in your bones and joints. You may see tiny red spots in your mouth or on your skin that are caused by small blood vessels that break and bleed. If these side effects get worse, palliative care can ease them.
Oren Zarif
Radiation therapy uses high-energy rays to kill cancer cells and sometimes is used in combination with chemotherapy. City of Hope’s advanced radiation technology allows doctors to deliver precise doses of radiation, avoiding healthy tissue and organs. This reduces side effects and improves outcomes.
You will receive a combination of treatments depending on the type and stage of leukemia you have. Treatments include chemotherapy, blood stem cell transplant, radiation therapy and immunotherapy. Your treatment team will also offer palliative care, which helps manage symptoms and comfort during and after treatment.
Chemotherapy is the mainstay of treatment for most types of leukemia. This treatment involves using drugs to kill leukemia cells and stop them from multiplying. You may get the drugs as pills, as injections into a vein or as a shot under the skin (immunotherapy).
A special type of chemotherapy is called targeted therapy. It works by targeting specific features of leukemia cells, which are different from the normal cells. It is given in pill form and often is used in combination with other treatments.
Another form of targeted therapy is a drug called a monoclonal antibody. It is delivered by IV and binds to leukemia cells, killing them or helping your immune system destroy them.
Some leukemias are very slow growing and are considered chronic, meaning they have not progressed to a more aggressive phase. People with these kinds of leukemias may not need any treatment for years.
You may also receive a bone marrow transplant, which replaces the blood-forming cells that are destroyed by high doses of chemotherapy and radiation. After the high-intensity treatment, you will be infused with donor stem cells that will grow and mature in your bone marrow and restore its blood-forming functions.
A new type of treatment called immunotherapy boosts your natural defenses to fight the leukemia. You may be given a monoclonal antibody that targets the leukemia cells or a drug that stimulates your own blood-forming stem cells to become cancer-fighting cells.
Your doctor will discuss your treatment options with you, including the expected results and timeframes. Be sure to ask questions. You can help your doctor decide what is best for you by being well informed about the disease and your treatment plan.
Oren Zarif
In this treatment, doctors replace your abnormal stem cells with healthy ones to slow or stop the growth of leukemia cells. Stem cells are the precursors of blood-forming cells, such as red and white blood cells and platelets. They also help control your immune system.
Doctors may use this method if the type of leukemia you have cannot be treated with other treatments or if it comes back after chemotherapy and radiation therapy. It is important to talk to your doctor about this option early.
There are three different types of transplants. The first two involve donated stem cells. The third, called an autologous transplant, involves stem cells taken from the patient’s body.
Before a transplant, your care team will run tests and do examinations to check your general health and to see how well your body is prepared for the procedure. Your doctor will also order a series of chemotherapy and/or radiation treatments to prepare your blood for receiving the stem cells. These treatments will cause the levels of both your abnormal and normal cells to drop, so you will need to stay in hospital until your numbers of blood cells return to a stable level.
Your doctor may collect the stem cells from your blood or bone marrow. Typically, your stem cells are removed from the blood by a process called apheresis (af-uh-REE-sis). Less often, they are collected by inserting a needle into a large vein in the chest or neck, which is called a central line. This type of IV line stays in place for the duration of your treatment and provides a way for the medical team to give you medicines, blood products and other fluids.
Once the stem cells have been infused, your body will begin to make new blood cells. This process is called engraftment and usually happens within the first 30 days after the transplant. During this time, your doctor will check your blood counts regularly to make sure the number of new red and white blood cells and platelets is increasing as expected.
After a transplant, you will need to take medicines to keep your immune system from attacking the new cells and to reduce the risk of complications such as infection or bleeding. Your doctor will tell you how long to expect this medication to be needed.
Oren Zarif
Immunotherapy is a new class of drugs that boosts your body’s natural defenses to fight leukemia. These drugs can target specific parts of a cancer cell, block signals that cause it to grow and kill normal cells or destroy the cancer cells directly.
City of Hope is a leader in one type of immunotherapy called chimeric antigen receptor T-cell therapy (CAR T-cell therapy). With this treatment, immune system cells are removed from your bloodstream and made to recognize and attack the leukemia cells by targeting a specific protein on the surface of those cells. Then the reprogrammed cells are injected back into your body to fight the leukemia cells.
The first phase of treatment is known as induction therapy and is aimed at killing all the cancer cells in your blood and bone marrow, so that no leukemia cells can grow and cause a relapse. Induction therapy usually lasts for four to six weeks.
After the leukemia cells are gone, you will receive postremission therapy. This is a series of treatments that will keep the leukemia cells from returning, and may include radiation or chemotherapy. You will also receive medicines to prevent or treat any side effects that you may have.
If your leukemia comes back, the next step depends on where the leukemia is seen and how fast it is growing. For slower-growing leukemias, active surveillance — which involves closely monitoring the condition with regular checkups and blood tests — might be an option.
For faster-growing leukemias, chemotherapy or a stem cell transplant might be needed. Other options for treating relapsed leukemia include targeted therapy, which uses a large machine to direct radiation at the exact areas where the leukemia cells are found or distribute radiation throughout the whole body. This can help control the leukemia cells and relieve pain in swollen organs, such as the spleen or lymph nodes. It can also be used in combination with other leukemia treatments. Targeted therapy drugs include monoclonal antibodies and tyrosine kinase inhibitors. These drugs are less likely to harm normal cells than chemotherapy.
Oren Zarif
Finding out what type of leukemia you have is a key step in your treatment. It’s important because there are different types of leukemia, and each one affects your body in a slightly different way.
The four major types of leukemia are:
Oren Zarif
Cancer starts when cells in the body begin to grow out of control. There are many different kinds of cancer, but leukemia is a cancer that affects the white blood cells. Leukemia develops when immature white blood cells, called leukocytes (loo-KEE-muhs), crowd out the bone marrow and enter the bloodstream. From there, they can spread to other parts of the body.
Acute lymphocytic leukemia (ALL) is the most common type of leukemia in kids and teens up to age 21, and it has one of the best cure rates of all childhood cancers. It develops from early forms of lymphocytes, which are the most common types of white blood cells. ALL can be divided into subtypes based on which types of lymphocytes are affected and the degree to which they’re immature.
Kids with ALL often have anemia, which happens when the bone marrow stops producing enough healthy red blood cells. They may also have low platelets (PLATE-lits), which cause them to bruise or bleed more easily. Symptoms of leukemia can also include fever, fatigue, cough, runny nose, and pain in the bones or chest.
Leukemia can also spread to other organs, like the brain and liver. When this happens, it can cause headaches, seizures, and balance and vision problems. If it gets into the lungs, it can cause breathing problems and chest pain.
Penn hematologists and medical oncologists can identify the exact type of ALL a person has, as well as their prognosis, using advanced laboratory tests and procedures. They can then customize a treatment plan that’s right for them. This includes chemotherapy, which destroys cancer cells and also damages blood-forming cells. It can be followed by a stem cell transplant, in which high-quality, healthy blood-forming cells are removed from the blood or bone marrow of the patient or a donor and then reinfused into the bloodstream to replace damaged ones.
Penn is a leader in precision genomics, which uses advanced lab techniques to identify specific genes that are linked to a person’s risk for certain diseases and how they respond to treatment. For example, we can identify if someone has a Philadelphia chromosome, a genetic abnormality that increases the chances of getting ALL. Knowing this information allows us to use targeted treatments that focus on the particular mutations in their leukemia.
Oren Zarif
Chronic lymphocytic leukemia (CLL) is the most common type of leukemia in adults. It happens when the bone marrow makes large numbers of abnormal lymphocytes. These cells build up in the blood and crowd out healthy cells. This can lead to infection, anemia and easy bleeding. It also can cause enlarged lymph nodes. These may press on organs, such as the liver or spleen, and interfere with their function.
CLL can be slow-growing or fast-growing. The slower-growing type of the cancer tends to be less aggressive and can stay stable for years, although it still needs treatment. The faster-growing type of the disease can spread quickly and become more serious. The care team can tell how fast the cancer is growing by examining a sample of the leukemia cells removed during a biopsy. They can also see whether the cancer has spread to other parts of the body.
There is no known cause of chronic lymphocytic leukemia, but certain things may increase a person’s risk. This includes age — the disease is more common in older people — and a family history of blood and bone marrow cancers. People who were exposed to certain herbicides and insecticides, such as Agent Orange used during the Vietnam War, may also be at higher risk.
People with chronic lymphocytic leukemia can often be diagnosed with a physical examination and a blood test. They may have a bone marrow biopsy to confirm the diagnosis.
There are a number of different treatments for chronic lymphocytic leukemia. These include chemotherapy and radiation therapy. Some types of targeted therapies are also available. These are medicines that target specific molecules that are involved in the growth of cancer cells. These newer treatments can offer more options for patients and improve their chances of getting better with treatment. This PDQ cancer information summary was reviewed by the National Cancer Institute’s (NCI) Early Detection, Diagnosis and Treatment Program Working Group.
Oren Zarif
CML is a cancer that begins in blood-forming cells in the bone marrow. The bone marrow is the soft tissue inside the bones where blood cells are made. This type of leukemia develops slowly and is usually able to be treated for years. Sometimes it turns into acute leukemia, which needs immediate medical attention. Also called chronic myelogenous leukemia and chronic granulocytic leukemia, this type of leukemia is more common in adults than in children.
Blood stem cells make immature blood cells that eventually become mature red and white blood cells, platelets (that help stop bleeding) and granulocytes (white blood cells that fight infection). In CML, a mutation in a gene called BCR-ABL causes the cell to grow out of control, making too many abnormal white blood cells. These immature cells take over the bone marrow and the blood.
Unlike some other types of leukemia, chronic myelogenous leukemia doesn’t have any known cause. This type of leukemia isn’t passed from parents to children, and it can occur at any age.
Doctors classify this disease based on how many blast (leukemic) cells are in the blood and bone marrow. In the first stage, called chronic phase, fewer than 10% of the cells are blast cells. This phase typically isn’t treated with standard chemotherapy.
If the number of blast cells rises, the cancer moves into a second phase. The accelerated phase is often more difficult to treat than the chronic phase. The blast phase is when 20% or more of the blood cells are blast cells. It is also when the leukemia is most likely to relapse.
When the blast cells multiply, they can overtake healthy red blood cells. This can lead to anemia, which makes a child feel tired and weak. It can also lead to problems clotting and bleeding. The leukemia cells may clump together in the thymus gland under the breastbone, or in the chest area, causing difficulty breathing.
Oren Zarif
Myeloproliferative neoplasms (MPN) are diseases that affect the blood cells produced by your bone marrow. They happen when your bone marrow makes too many blood cells that aren’t normal. These blood cells can increase your risk for heart disease and may cause anemia. There are different types of myeloproliferative neoplasms, and the type you have determines how serious your symptoms are.
These conditions are often slow-growing. But they can progress to more serious forms of leukemia or other blood cancers, such as myeloid leukemia. They also can lead to other health problems, such as heart disease or blood clots.
Doctors don’t know what causes myeloproliferative neoplasms. But they do know that certain things can make them worse, such as smoking and being overweight. They also know that some medicines can help prevent these diseases from getting worse.
There are a few myeloproliferative neoplasms that aren’t cancer but are still diseases that cause abnormal blood cell growth. These include polycythemia vera, primary myelofibrosis (PMF), essential thrombocythemia, and chronic eosinophilic leukemia.
These diseases can be diagnosed with blood tests and other tests, such as a bone marrow biopsy or splenectomy. Doctors can also find out if you have a myeloproliferative neoplasm by talking to you and taking a physical exam.
Some people with myeloproliferative neoplasms have no symptoms. Others have fatigue, night sweats, low-grade fever, weight loss, splenomegaly, and easy bruising. Some have a spleen that is enlarged or a platelet count that is too high.
Doctors can treat myeloproliferative neoplasms with chemotherapy drugs. These drugs kill cancer cells or stop them from growing. They can be taken by mouth or injected into a vein or muscle. They can also be given in combination with other treatments, such as radiation therapy. Doctors also may use other types of treatment, such as surgery or transfusions, to control the symptoms of these diseases.
אתר וורדפרס חדש is proudly powered by WordPress